Beyond Being “Neat”: The Reality of Obsessive-Compulsive Disorder (OCD)
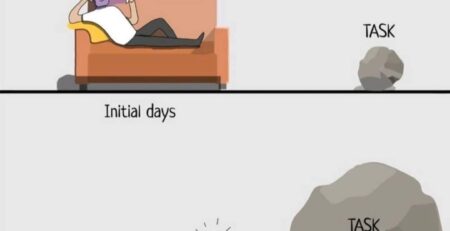
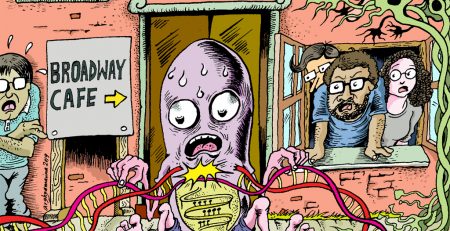
Obsessive-Compulsive Disorder (OCD) is a chronic condition characterized by obsessions (unwanted, intrusive thoughts) and compulsions (repetitive behaviors performed to reduce anxiety). It is not simply a desire for cleanliness; it is a disabling cycle of doubt and ritual. Recent studies suggest a prevalence of nearly 3% in certain Indian populations, with onset often in young adulthood.
Common OCD Themes in India
-
Contamination: Fear of dirt, germs, or “impure” substances, leading to excessive hand washing or bathing.
-
Pathological Doubt: Repeatedly checking locks, gas cylinders, or switches.
-
Religious/Blasphemous Obsessions: Intrusive bad thoughts about deities, leading to excessive praying or apology rituals.
-
Symmetry: Need for items to be arranged in a specific order.
The Role of Family: “Accommodation” In the Indian family context, relatives often “accommodate” the patient’s OCD to reduce their distress (e.g., buying extra soap, opening doors for them). Research shows that high family accommodation can actually worsen OCD severity. Treatment often involves educating the family to support recovery rather than the ritual.
Treatment Strategies
-
ERP Therapy: Exposure and Response Prevention (ERP) is the most effective psychotherapy. It involves facing the fear (e.g., touching a doorknob) without performing the ritual (e.g., not washing hands).
-
Pharmacotherapy: High-dose SSRIs are often required for OCD management.
-
Yoga as Adjunct: A study from NIMHANS and other Indian institutes suggests that yoga-based interventions can significantly reduce OCD symptom severity when added to medication.
Frequently Asked Questions (FAQ)
Q: Is OCD a form of “madness”? A: No. Patients with OCD usually have “insight,” meaning they know their thoughts are irrational but feel powerless to stop them.
Q: Can Ayurveda help OCD? A: Ayurveda (e.g., Brahmi, Ashwagandha) acts as a wellness adjunct to improve cognitive function and reduce stress, but it should not replace standard psychiatric care for clinical OCD.